The Vaginal Microbiome

What Every Woman Should Know (But Rarely Hears About)
As you go about your day—your running errands, finishing a workout, or even lounging poolside in a swimsuit—there’s a remarkable community of microorganisms quietly working to keep you healthy below the belt.
You probably haven’t thought much about it. I hadn’t either, even working in women’s health. But recent research is shedding light on just how crucial the vaginal microbiome is—not just for preventing infections, but also for supporting fertility and lowering the risk of things like STIs and preterm birth.
Of course, new discoveries also bring new questions—and a wave of wellness products promising to "balance your flora." But it’s not always clear what’s helpful and what’s just hype. Do you really need that probiotic suppository you saw on Instagram? Could something be off even if you feel fine?
Even everyday things like sitting in a wet swimsuit too long can create the warm, moist environment that promotes bacterial growth near the urethra. While wearing a wet suit doesn’t cause UTIs directly, it can increase your risk—especially if other factors are in play.
So let’s get into it. This post is your guide to understanding what the vaginal microbiome is, why it matters, what can throw it off, and how to support it. Because once you know how it works, you’ll never think of it as an afterthought again.
What Is the Vaginal Microbiome—And Why It Matters
All women have a vaginal microbiota, but every woman’s vaginal microbiota is different.
- For most women (and in contrast to the gut microbiota) the vaginal microbiota is balanced when its diversity is low (c. 200 bacterial species) and when lactobacilli – rod-shaped bacteria – predominate.
- To date, five main types of vaginal bacterial communities have been described:
- four are dominated by lactobacilli (Lactobacillus crispatus, L. gasseri, L. iners, or L. jensenii),
- one characterized by a low content or absence of lactobacilli
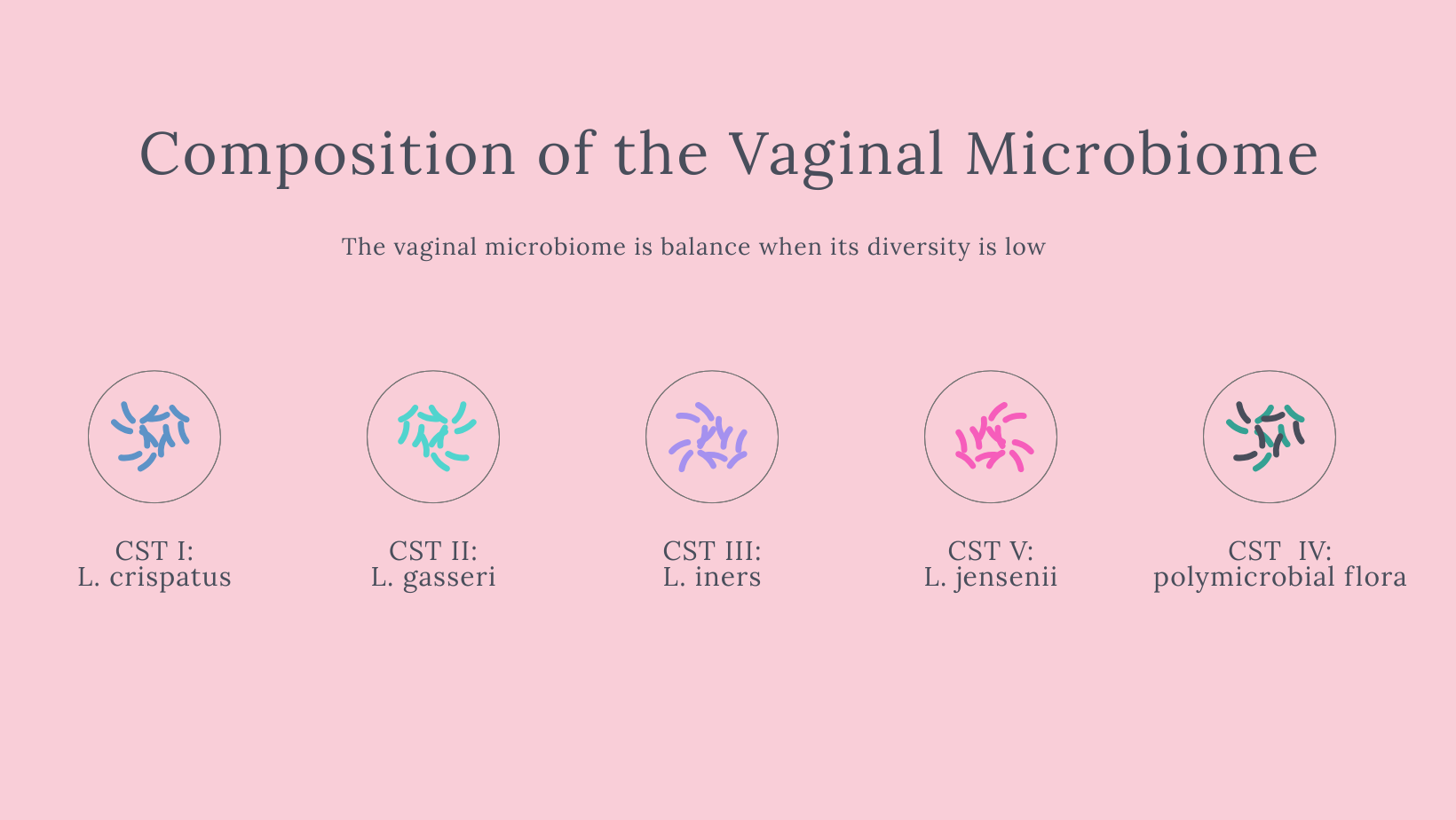
Scientists classify the vaginal microbiome into Community State Types (CSTs):
- CST I: Dominated by L. crispatus
- CST II: Dominated by L. gasseri
- CST III: Dominated by L. iners
- CST V: Dominated by L. jensenii
- CST IV: Diverse anaerobic bacteria, low Lactobacillus—linked with bacterial vaginosis (BV) and dysbiosis
These bacteria are health heroes. They produce lactic acid, hydrogen peroxide, and bacteriocins, which lower pH, fight off pathogens, and support immune function. This acidic environment (~pH 3.8–4.5) helps prevent infections, supports fertility, and protects against complications during pregnancy.
A Lactobacillus-dominant microbiome is generally associated with better health outcomes. When this balance shifts (e.g., more anaerobes like Gardnerella or Prevotella), infection risk increases.
What Disrupts the Balance?
Unfortunately, there are many everyday factors that can throw this delicate ecosystem off:
- Hormonal fluctuations (menstrual cycle, pregnancy, menopause)
- Antibiotic use
- Hormonal birth control
- Sexual activity and new partners
- Hygiene products (douching, scented washes)
- Stress, poor sleep, and high-sugar diets
Some of these are unavoidable. But many can be managed once we’re aware of their impact. This isn’t about perfection—it’s about curiosity, care, and informed choices.
Signs of Imbalance
Your body usually sends signals when something’s off. Signs of a disrupted vaginal microbiome may include:
- Recurring bacterial vaginosis (BV) or yeast infections
- Unusual discharge, odor, or discomfort
- Vaginal itching, irritation, or dryness
If any of these sound familiar, you’re not alone. And you’re not doing anything wrong.
What Supports a Healthy Vaginal Microbiome?
Gentle care practices:
- Skip douching and scented products
- Choose breathable cotton underwear
- Be mindful of sexual health practices
- Manage stress and prioritize rest
Food and gut support:
- Eat fiber-rich, plant-forward meals
- Include fermented foods like yogurt and kefir
- Support gut health—because the vaginal and gut microbiomes are closely linked
Period hygiene:
- Change pads or tampons regularly
- Use warm water and mild soap—nothing fancy needed
How the Vaginal Microbiome Changes Across Your Life
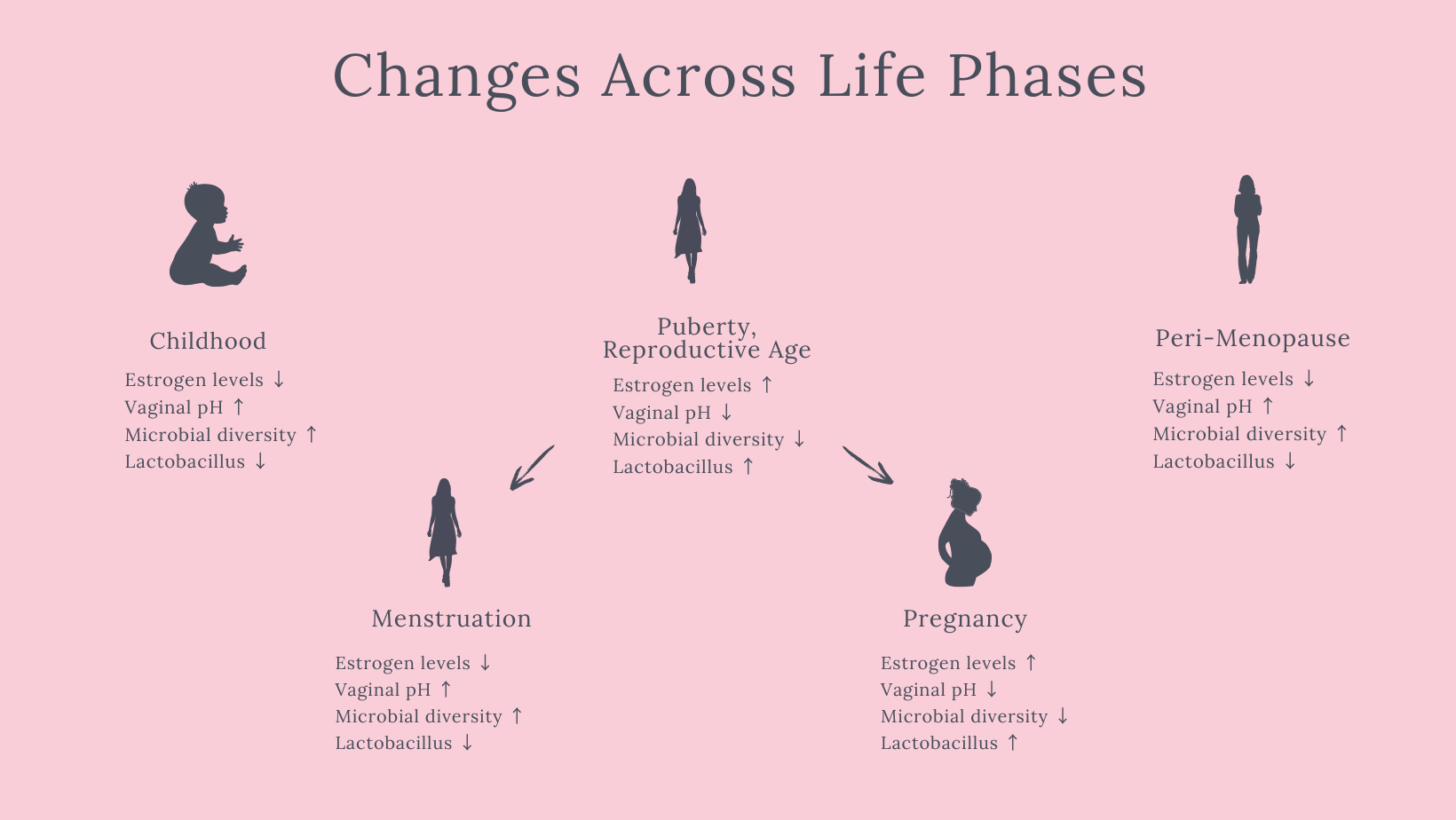
Our body evolves over time—and so does your vaginal microbiome. From childhood through menopause, hormonal shifts influence microbial composition.
- Childhood: Low estrogen levels mean a diverse, polymicrobial vaginal environment.
- Puberty & Reproductive Years: Rising estrogen encourages Lactobacillus dominance, creating a more protective, acidic environment.
- Menstruation: Blood raises vaginal pH, reducing Lactobacillus temporarily and increasing diversity. The microbiome typically resets post-menses.
- Pregnancy: Estrogen surges lead to a more stable, Lactobacillus-rich microbiome—thought to protect both mother and baby.
- Postpartum: The microbiome shifts again as hormones readjust.
- Menopause: Declining estrogen levels reduce Lactobacillus dominance, increasing pH and the potential for infections or irritation.
Each phase of life brings its own microbial rhythm. Understanding these shifts can help us care for our bodies with more confidence, compassion, and support.
Where the Research Is Going—and Why It Matters
We’re only beginning to understand how vital this ecosystem is. Researchers are now uncovering connections between the vaginal microbiome and everything from fertility outcomes and pregnancy complications to chronic pelvic pain and gynecologic cancers.
Some strains of Lactobacillus are being studied for their anti-inflammatory and immune-supportive properties, and scientists are working to develop diagnostic tools that could one day personalize care based on your unique microbiome profile.
It’s a fast-moving field, full of potential. And while there’s still a lot we don’t know, one thing is clear: this tiny ecosystem plays a much bigger role in our overall health than we’ve been taught.
Conclusion: Know Your Microbiome, Know Your Body
I didn’t grow up learning about my vaginal microbiome—and chances are, you didn’t either. But that’s changing. And it starts with conversations like this one.
This tiny community inside you is powerful. It deserves care, respect, and attention—just like every other part of your health.
The more we normalize learning about it, the less confusing and intimidating it becomes. And the more we can lean into care—not fear, shame, or guesswork.
Here’s to making the invisible visible—and giving our bodies the informed care they’ve always deserved.