Why Inflammation Could Be the Missing Link in How You Age

You’re in your mid-30s or early 40s. You’re juggling work, home, maybe kids — and doing your best to stay healthy. You’ve figured out how to sneak in some movement, keep a balanced-ish diet, and prioritize sleep when you can. But something still feels… off.
What if the culprit isn’t just “getting older” — but inflammation?
Let’s talk about what it really means, how it uniquely affects women, and why understanding it could be the key to not just living longer, but aging well.
💥 Inflammation 101: Friend, Then Foe
Inflammation isn’t all bad. It’s your body’s natural response to injury or infection — part of your immune defense squad. That’s acute inflammation, and it helps you heal.
But chronic low-grade inflammation?
That’s a different story. It’s subtle. It simmers. And over time, it can damage tissues, accelerate aging, and increase your risk of diseases like:
- Cardiovascular disease
- Alzheimer’s disease
- Type 2 diabetes
- Osteoporosis
- Certain cancers
❤️🩹 Why Inflammation Hits Women Differently
Reproductive life span matters
Here’s something fascinating: research shows that women with a longer reproductive life span (from first period to menopause) tend to have lower levels of inflammation later in life.
Even though ovulation itself is a mini inflammatory event, more years of ovulation seem to protect you. Studies like the Nurses’ Health Study have found that women with longer reproductive spans have lower CRP levels (a key inflammation marker), even when controlling for body weight, exercise, and diet.
So yes — your menstrual history can play a role in your long-term health.
Lower baseline inflammation
Compared to men, women generally have lower baseline inflammation — especially in older age groups. This may help explain why women live longer. But that doesn’t mean you’re in the clear.
Once menopause hits, inflammation levels rise. That’s when risks increase for:
- Bone loss (hello, osteoporosis)
- Joint pain (osteoarthritis)
- Frailty and muscle loss
This transition isn’t just hormonal; it’s immunological- meaning it affects how your immune system functions and responds to stress, injury, or aging.
Biomarkers: The Signals You Don’t Want to Miss
Not all inflammation shows up as pain. Here are some key biomarkers you can ask your doctor to check:
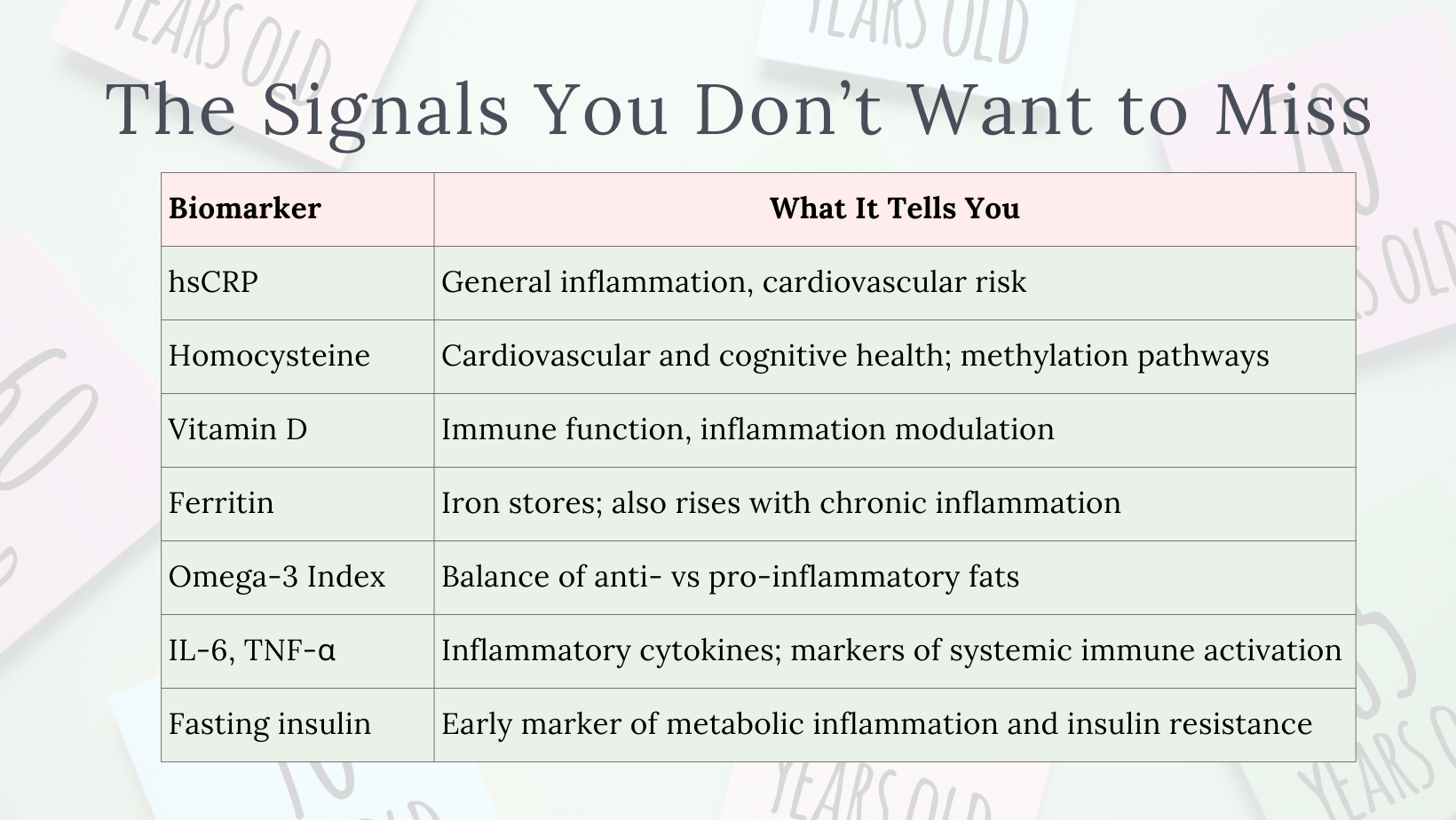
If you’re starting to feel more inflamed than you used to, it’s not all in your head — and it may show up in your bloodwork before your symptoms do.
Some women also benefit from advanced testing, including inflammatory cytokines (like IL-6, TNF-α) or the ratio of omega-6 to omega-3 fatty acids, especially if they’re navigating perimenopause, autoimmune symptoms, or fatigue that doesn’t resolve with rest.
How to Cool the Fire, Daily
You don’t need a prescription to start dialing inflammation down. Here’s what works — and why it matters more than ever in your 30s and 40s.
🥗 Eat anti-inflammatory (most of the time)
Think plants, omega-3s, and real food.
- Eat: leafy greens, berries, olive oil, nuts, fatty fish, turmeric
- Limit: processed foods, excess sugar, alcohol
- Bonus: eating consistently (without skipping meals) helps reduce blood sugar spikes that drive inflammation.
💤 Protect your sleep like it’s sacred
7–9 hours of good-quality sleep supports inflammation regulation, hormone balance, and immune repair.
Sleep disruptions raise CRP, and women are more prone to sleep problems in perimenopause — so don’t brush off those restless nights.
🏃♀️ Move — but don’t overtrain
Exercise helps lower inflammation, but too much high-intensity without rest can backfire.
Mix in walking, strength training, yoga, or mobility work. It’s about consistency, not perfection.
🧘♀️ Manage stress like your life depends on it (because it kind of does)
Chronic stress = chronic inflammation.
Even 5–10 minutes a day of deep breathing, journaling, or simply doing nothing can help cool your system.
Try to reframe “self-care” as something that includes boundaries, saying no, and reclaiming small moments of peace.
🔮 The Future: Can We Target Inflammation to Live Longer?
Science is catching up to what many women feel:
- Inflammatory proteins like IL-11 have been targeted in animal studies, extending healthspan (not just lifespan).
- Centenarians (especially healthy women over 100) often show remarkable control over systemic inflammation, suggesting it’s not just genes — it’s lifestyle, immune resilience, and stress response.
As therapies evolve, you may one day see precision inflammation-targeted treatments. But right now, your daily choices are your most powerful medicine.
💡 Final Takeaways
Your reproductive history, lifestyle, and stress levels all influence it.
Testing key markers can give you insight. But action beats information. Eating well, sleeping enough, managing stress, and moving intentionally are powerful tools — especially in this stage of life. Longevity is about resilience, not perfection. It’s how you care for yourself daily that adds up.
🌱 Aging Isn’t About Fighting Time — It’s About Supporting Your Body
If you’re pursuing longevity, it’s not just about living longer — it’s about living well. A vibrant, meaningful life that includes joy, connection, and pleasure. So don’t deprive yourself of everything that makes life sweet. An anti-inflammatory lifestyle isn’t about rigid rules or restriction. It’s about choosing what supports your health most of the time, and making space for what delights you, too.
You’re not broken. You’re just in a season of life where your body is asking for different things. Listening to that — and giving it what it needs — is the best longevity strategy there is.
You don’t need to overhaul your life overnight. But you can choose one small thing today that cools the fire.
Less burn, more glow.
That’s the path to aging well — inside and out.
