Why Your Stress Response Changes Throughout the Month

If you've been around here for a while, you know I'm all about helping women make sense of their hormones. I’ve already written about how stress shows up on your to-do list—especially when cortisol, your main stress hormone, is running the show behind the scenes. I also shared how to make sense of hormone testing, and how stress can sneakily disrupt estrogen, progesterone, and even thyroid hormones.
But today, we’re zooming in on something that doesn’t get nearly enough attention:
👉 how your cortisol levels shift naturally across your menstrual cycle—and what that means for your energy, stress resilience, mood, and overall well-being.
Because guess what? Your stress response doesn’t run on the same settings all month long. And when we ignore that? We risk pushing through when we should be restoring.
Let’s dig into the details.
First, a Quick Cortisol Recap
Cortisol is often called the “stress hormone,” but it’s really more like your body’s built-in energy and survival manager. It’s produced by your adrenal glands and helps regulate:
- Blood sugar and energy
- Immune responses
- Sleep-wake cycles
- Inflammation
- Mood and focus
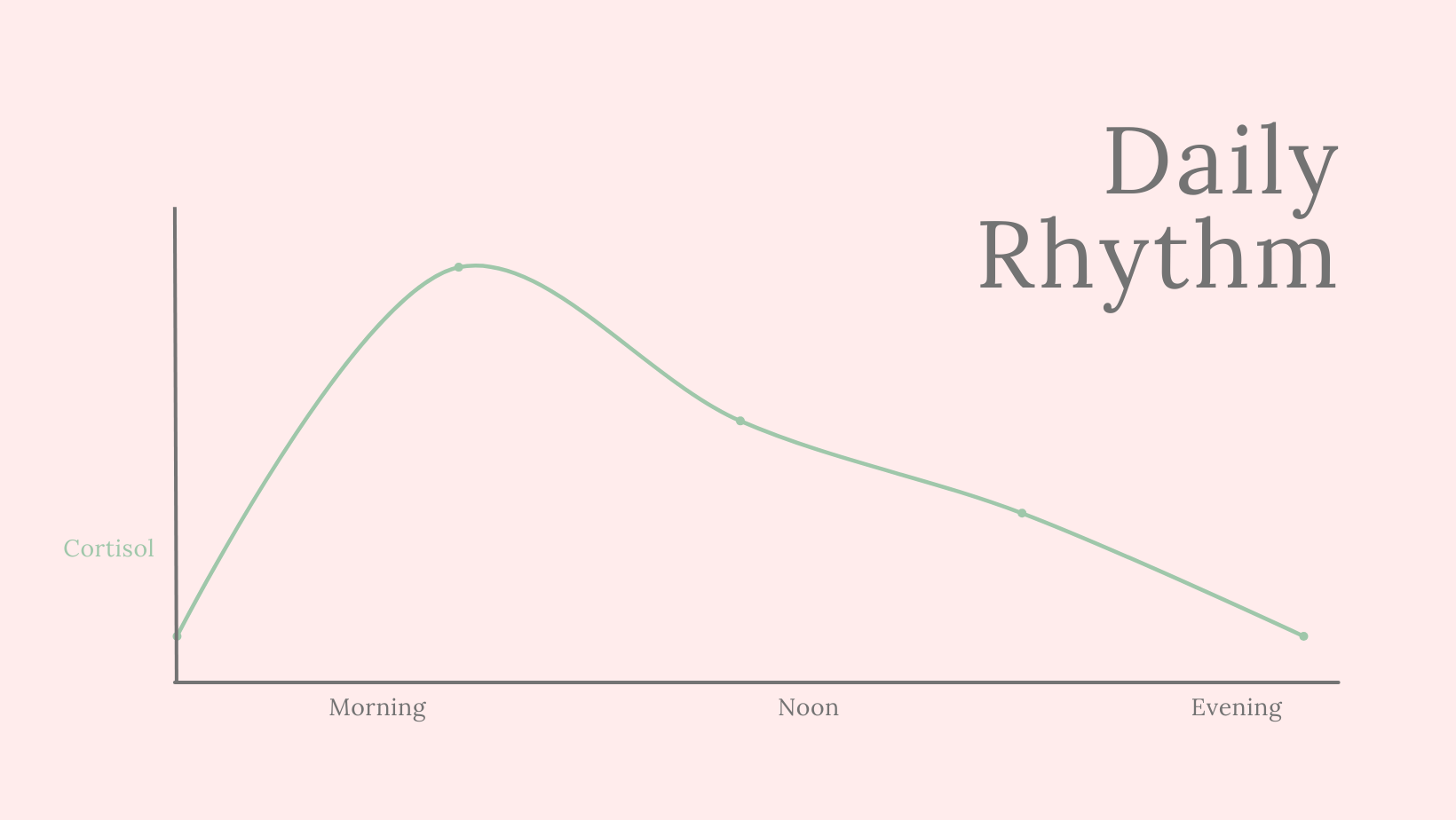
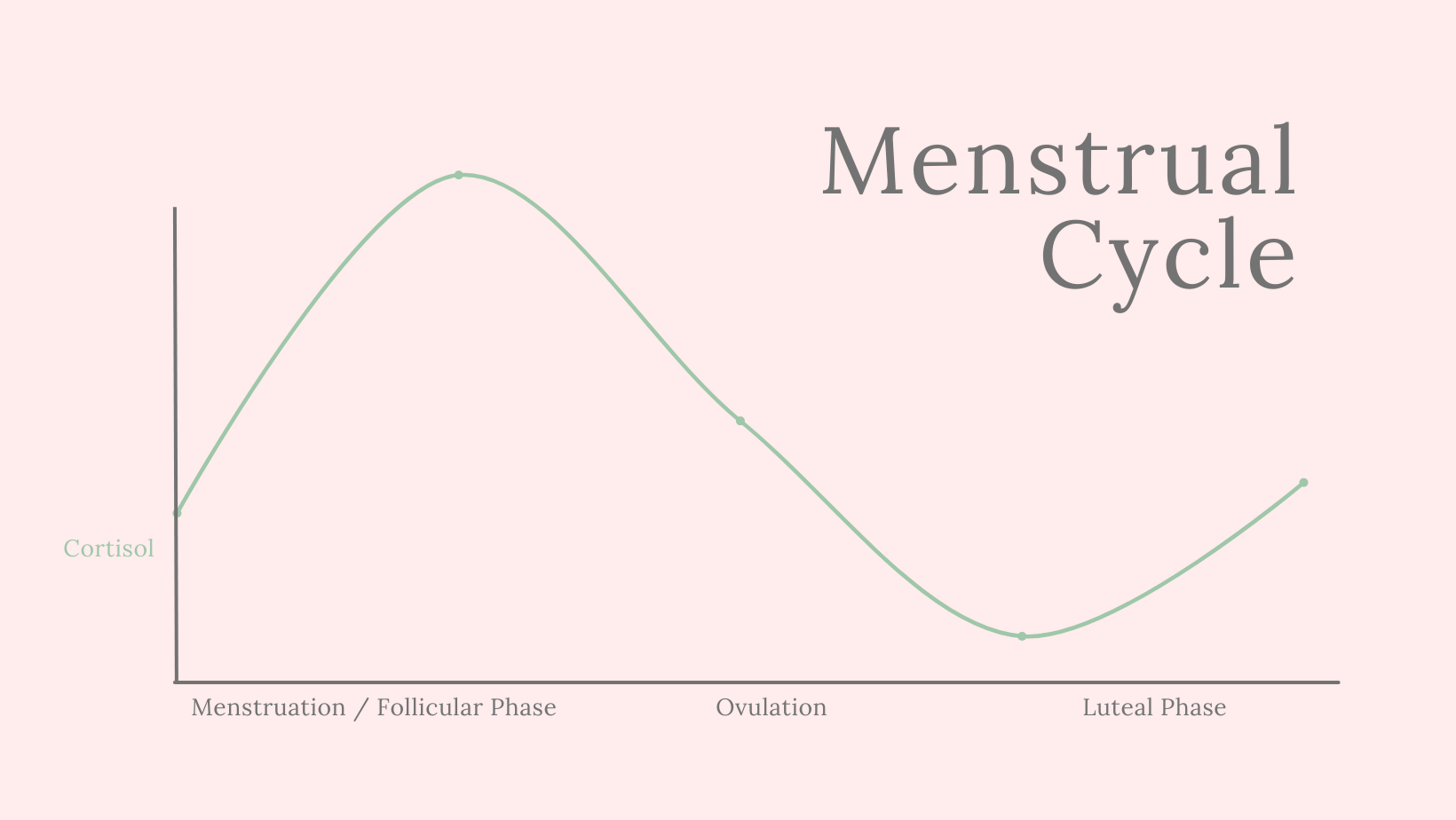
It follows a daily rhythm (peaking in the morning, tapering off in the evening), but also a monthly rhythm—especially in women. And that's where your menstrual cycle comes in.
Meet the Players: Your Cycle & Cortisol
Your menstrual cycle is more than just “on your period” or not. It includes fluctuating levels of estrogen and progesterone, which directly impact how much cortisol you produce and how reactive you are to stress.
Here’s a closer look at what’s happening in each phase:
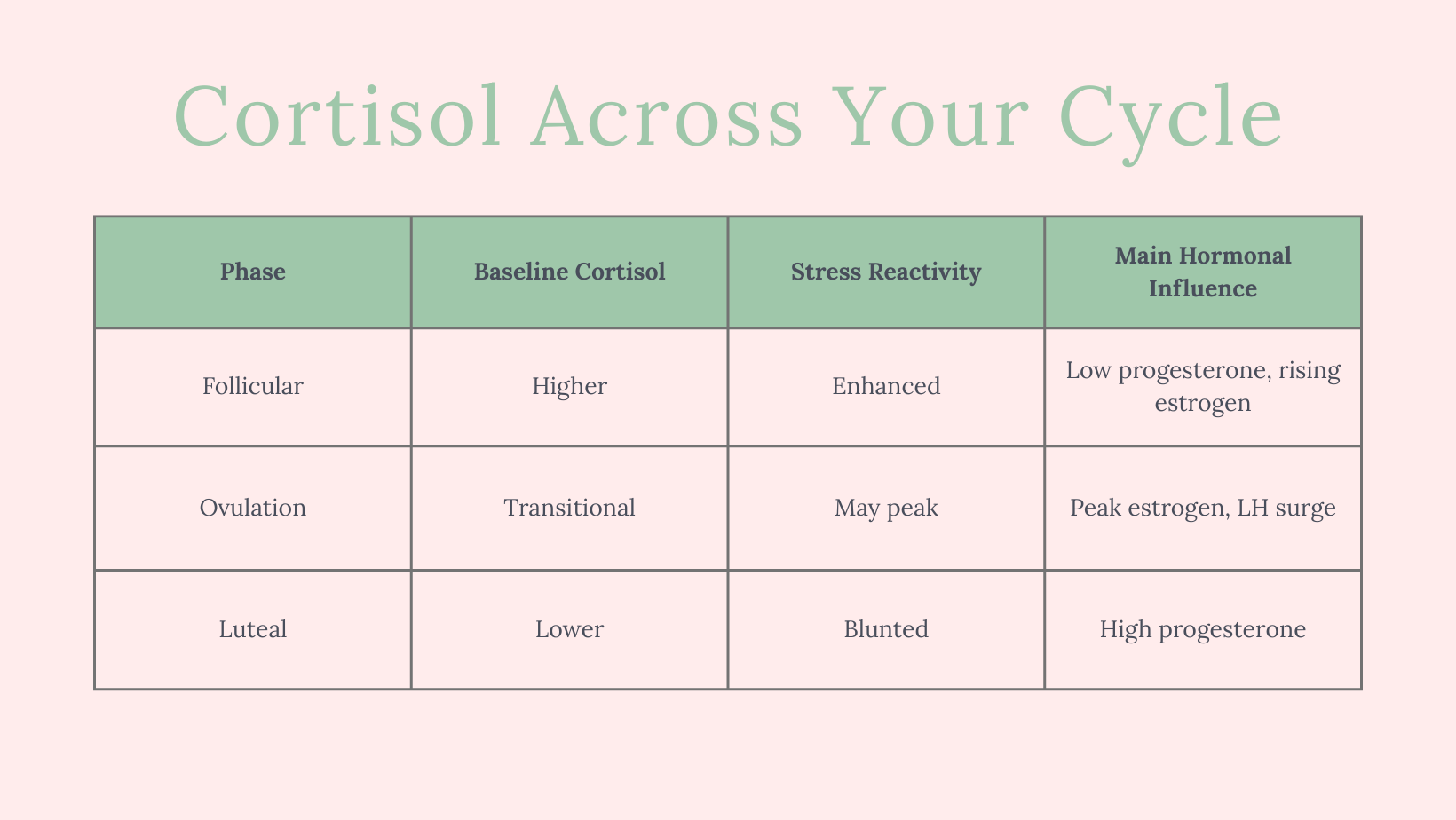
🌱 Follicular Phase (Days 1–14): Your High-Energy Window
- Dominant hormone: Estrogen (rising)
- Cortisol baseline: Higher
- Stress reactivity: Enhanced
This is the phase that starts on day 1 of your period and ends at ovulation. Estrogen is climbing, progesterone is still low—and your cortisol baseline tends to be higher. That might sound bad, but it’s actually super functional.
📈 This is your go-get-it phase. Cortisol helps keep you energized, focused, and mentally sharp. It's part of what makes this a great time for high-intensity workouts, social events, and deep work projects.
Studies confirm that circulating cortisol is significantly higher during the follicular phase than the luteal phase. It’s thought this helps support alertness and energy as your body prepares for ovulation.
💡 Pro tip: You might also notice you feel more sensitive to stress during this phase. Lab research shows women in the follicular phase have a stronger cortisol response to stress compared to the luteal phase.
🌸 Ovulation (~Day 14): The Turning Point
- Dominant hormone: LH surge, peak estrogen
- Cortisol baseline: Transitional (may peak)
As estrogen hits its peak and you ovulate, cortisol may rise too. It’s a bit of a wild card moment: for some women, it feels like a powerful surge of confidence and clarity. For others, especially if they’re underslept or overworked, it can tip into anxiety or agitation.
The key here is awareness—your body is peaking in many ways. Make sure you're fueling well and allowing time for rest between all the productivity.
💤 Luteal Phase (Days 15–28): Your Wind-Down Mode
- Dominant hormone: Progesterone
- Cortisol baseline: Lower
- Stress reactivity: Blunted
After ovulation, progesterone takes the lead. This is a calming, soothing hormone—and it brings cortisol down with it.
Progesterone and its metabolite, allopregnanolone, activate GABA receptors in the brain. This creates an inhibitory, anti-anxiety effect that naturally suppresses cortisol output by calming the HPA axis (the system that governs your stress response).
This might sound like bliss (and for some women, it is!), but it can also come with:
- Lower energy
- Brain fog
- Emotional sensitivity
- Reduced motivation
Your body is literally telling you: "Hey, can we not push today?"
This is not the time to start a new HIIT routine or work late every night. It’s a time for gentle movement, sleep support, and maybe scheduling fewer social obligations.
Mechanisms at Play: Why Cortisol Changes
Let’s get nerdy for a second:
- HPA and HPG Axis Cross-Talk
Your stress and reproductive hormone systems (aka HPA and HPG axes) are constantly talking to each other. When one goes haywire, the other feels it. - Estrogen & Progesterone Effects
Estrogen can either stimulate or inhibit cortisol, depending on which receptors it activates. Progesterone and its calming metabolites almost always suppress cortisol. - Corticosteroid-Binding Globulin (CBG)
Estrogen increases the amount of CBG in your blood, which binds cortisol. This affects total cortisol levels—but not necessarily the “free,” active form.
So… What Can You Do With This Info?
Start working with your cycle, not against it.
🗓 Plan your calendar to match your hormonal strengths
💪 Train smarter, rest better
❤️ Show yourself compassion when energy dips or emotions rise
🧠 Notice patterns in your stress levels, and track them across your cycle
This is how we stop blaming ourselves for being “too emotional,” “too tired,” or “not motivated enough.” Your hormones aren’t working against you—they’re guiding you.
And when you learn to tune into them? Life gets a whole lot smoother.
Want to Learn More?
I wrote more about cortisol in everyday life in this post:
👉 Cortisol Levels and Your To-Do List
And if you're wondering about hormone testing or want to dig deeper into how stress affects the whole hormonal harmony, there's more coming soon. 💌
Until then—track your cycle, watch how your body responds to stress, and be gentle with yourself. You're not a robot. You’re a cyclical, brilliant, ever-changing woman.